Over the past month I have been closely tracking my blood glucose while collecting and measuring strategies to improve control. I’ve found a few tricks that allow me to avoid glucose excursions and react effectively when I make mistakes.
Bolus Before You Eat
Anybody with T1D will tell you that getting meal boluses right is hard. Day to day my body’s insulin response varies, carbs are hard to estimate, and insulin doesn’t kick in right away. The “rapid acting” insulin I use isn’t that rapid at all, with 1-2 hours before peak effectiveness and a multi-hour tail.

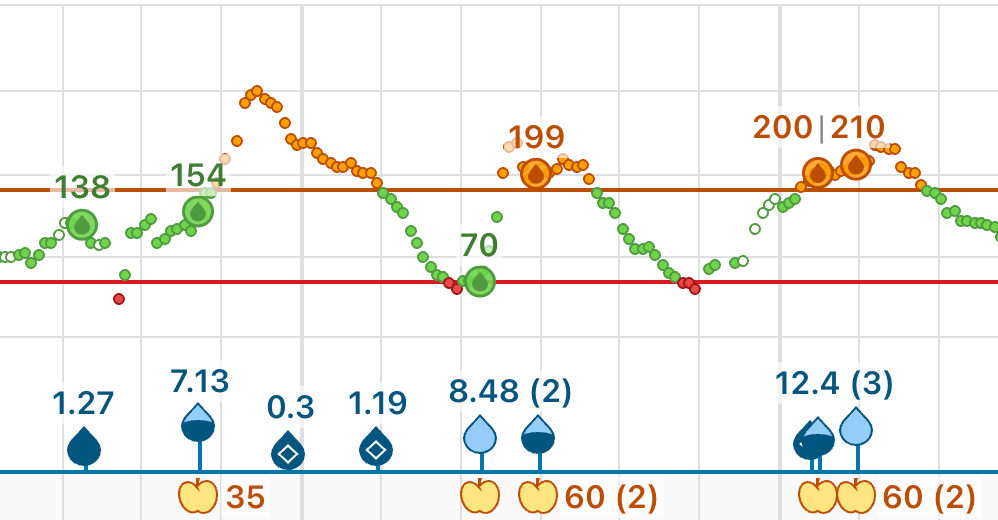
The insulin onset delay makes excellent glucose regulation difficult. Notice that even when insulin is administered at mealtime, postprandial (after meal) glucose can rise followed by a low several hours later.
A great strategy to avoid the mealtime rollercoaster is to pre-bolus, giving insulin 15-30 minutes before eating, or longer before if pre-meal glucose is high. A trace with “pre-bolusing” might look more like this.
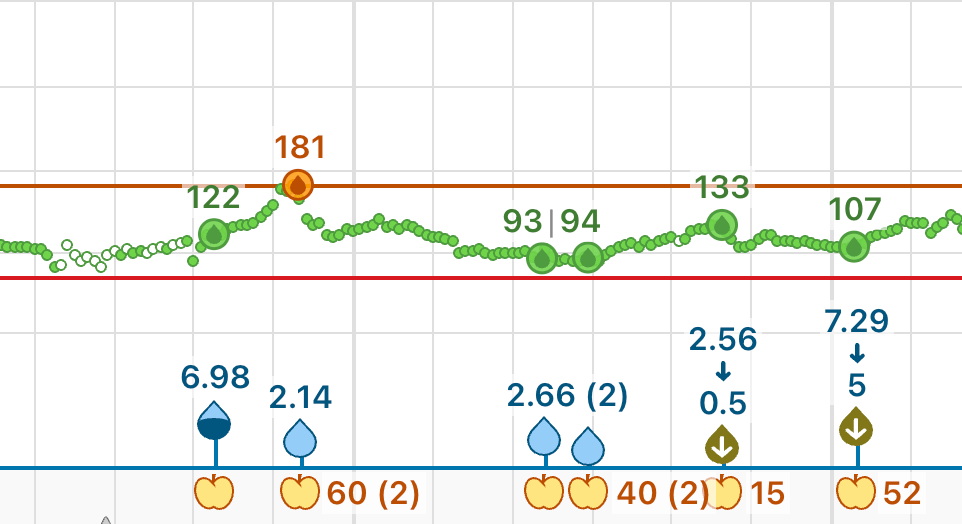
Notice how the bolus comes before the glucose rise, and how the overall line is flatter.
Use “Exercise Snacks” to Correct Hyperglycemia
Let’s say you’ve bolused and eaten a large, carb-rich meal. All too often, even with pre-bolusing and decent carb estimation, your glucose will rise and stay stubbornly high for hours after the meal. Let’s say you pump in a large amount of insulin to bring the glucose down. Insulin will only kick in after half an hour or so, and will peak after the food has been digested. This will usually lead to a low in 2-4 hours.
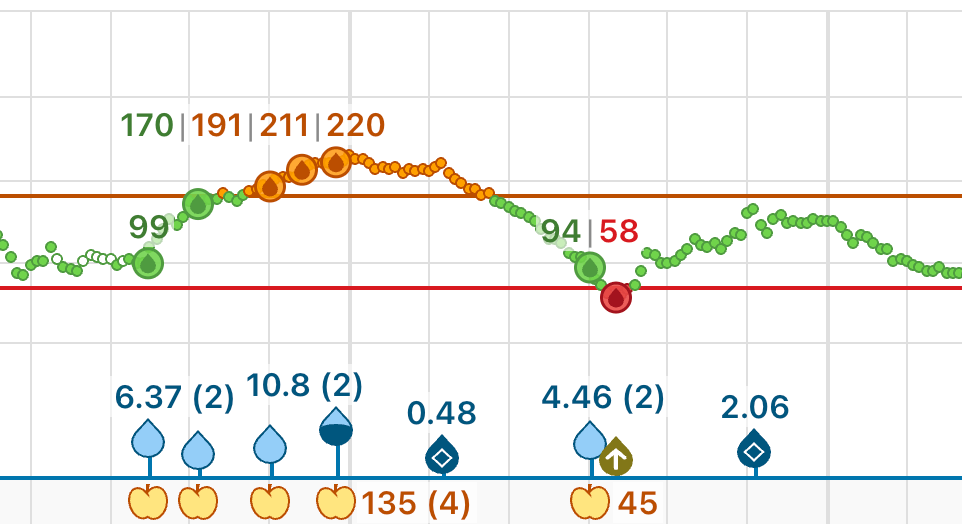
Rather than delivering a large bolus and waiting, let’s say you do something to temporarily increase insulin sensitivity. I’ve noticed certain medium intensity activities always send my number low, so let’s use these to transiently sensitize ourselves to the insulin we already have on board. Snow shoveling*, wood splitting*, gardening, hitting golf balls into a backyard net and going for a brisk walk or jog all do wonders to bring my number down quickly.
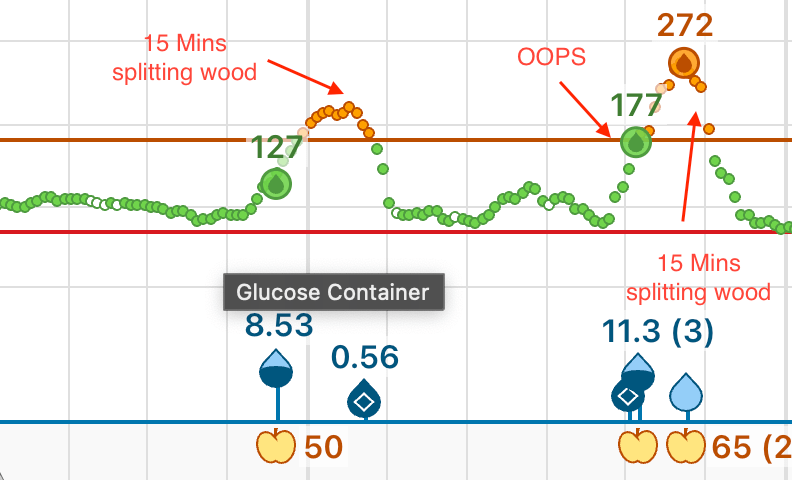
In this trace, you can see how short duration activity (in this case splitting wood) quickly brought down my glucose without requiring more insulin and without the resulting hypoglycemia. Even with a completely forgotten bolus like in the second spike, the glucose comes down within an hour.
Not everybody has a golf net in the backyard, never mind a pile of firewood to be split. Regardless, a brisk walk, pushups, air squats or any other medium to high intensity short duration exercise can help your muscles absorb the elevated glucose in your bloodstream. It’s also a chance to embrace being the weird person doing air squats in the airport or at work.
* You can tell I’m writing this post in rural Massachusetts from my choice of esoteric activities like snow shoveling and wood splitting.
Improve Insulin Sensitivity
The topic of insulin sensitivity and metabolic health spans entire academic careers so it’s impossible to cover exhaustively. Regardless, I’d like to share a few tips that have personally helped me. Overall, I’ve found that common advice about food and exercise rings true. Eating a diet with lots of vegetables and fiber as well as a balanced mix of unsaturated fats and slow carbohydrates results in long term insulin sensitivity and better glucose control. While I’m still collecting evidence, I have anecdotally found that meals with excessive saturated fat result in insulin resistance. Exercise, especially long duration cardio like running, walking, cycling and cross country skiing result in improved insulin sensitivity during the activity and across the following day or more. Sleep interruption or deprivation causes insulin resistance. Stress causes insulin resistance. These are topics I want to investigate and quantify in future blog posts once I have collected more data, but I’m pretty confident about the directionality and causality of these inputs on insulin sensitivity.
Ultra Rapid Acting Inhaled Insulin (Afrezza)
Inhaled insulin is delivered directly to the bloodstream via the lungs, meaning it begins working almost immediately and is mostly cleared from the system after an hour. This makes it ideal for handling very high glycemic index foods as well as correcting stubborn hyperglycemia without a resulting low 2-4 hours later. See the follow chart comparing the action profiles of Afrezza (TI) and rapid acting insulin (RAA).

I will be trying Afrezza to rapidly correct hyperglycemia and report on my experience in a future post.
GLP1 Receptor Agonists
GLP-1 receptor agonists like Semiglutide (Ozempic) and Tirzepitide (Mounjaro) can slow gastric emptying (reducing postprandial highs), reduce cravings for high glycemic index foods and potentially, though possibly not directly, improve insulin sensitivity. There is existing work investigating GLP-1 receptor agonists in T1D with promising results. I have never tried this class of medications so I cannot add anything to the discussion, but it’s worth noting that they may provide a powerful tool for some type 1 diabetics.
Conclusion
Overall, leading a healthy lifestyle with lots of physical activity, a balanced diet and well planned meals has dramatically improved my glycemic control. Strategically timed physical activity can work wonders to reduce the duration and magnitude of hyperglycemia. I am still investigating the exact correlations between various foods and insulin sensitivity, as well as other tools like Afrezza. This post outlines my current understanding of the effect of lifestyle factors and medications on glycemic control. I will continue to share as my understanding changes while I collect more data and try more strategies.
Leave a comment